Reducing Avoidable Emergency Department Transfers at an Inpatient Behavioral Health Hospital
Overview
The Med-X Consulting Team implemented a novel multidisciplinary intervention at a 270 bed behavioral health hospital in North Carolina.
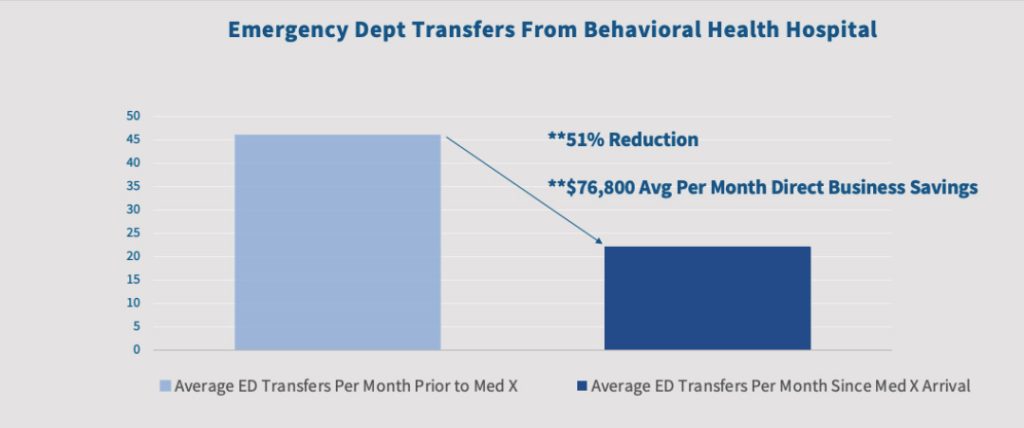
This intervention resulted in a greater than 50% reduction in emergency room (ER) transfers within three months, which equates to an average of $76,800 in direct savings per month for the behavioral health hospital. This reduction has been maintained for over two years.
The intervention involved staff education, protocol development, and enhanced medical capabilities, significantly improving the management of medical concerns within this behavioral health hospital. This case report details the intervention strategies, significant outcomes achieved, and the potential for broader application in similar healthcare environments.
Introduction
These transfers add pressure to the healthcare system and interrupt behavioral health care treatment, leading to potentially increased levels of emotional and physical distress for the patients2-3 The transfers are also a costly expense passed directly to the psychiatric facilities.
While various studies have explored models to reduce ER transfers from skilled nursing homes and rehabilitation settings4, there is a lack of research focused on reducing ER transfers from acute inpatient behavioral health facilities and their impact on patient health. Recognizing this gap, a North Carolina behavioral health hospital partnered with Med-X Consulting to develop and implement strategies aimed at minimizing avoidable ER transfers.
Solution
The Med-X consulting team conducted a thorough analysis of the behavioral health hospitals’ current operating structure, policies, and procedures. Additionally, in partnership with their current care team data was collected, historical base lines were established and key performance indicator goals were set. From this analysis, Med-X implemented a multidisciplinary approach to decrease ER transfers. Key strategies included:
- Education and Training: All nursing staff underwent comprehensive training to manage acute medical concerns effectively within the behavioral health hospital. This included recognizing early signs of medical issues and utilizing new protocols to address them promptly.
- Protocol Development: Several protocols were developed to streamline the identification and management of acute medical issues. These protocols emphasized early detection and intervention, aiming to prevent conditions from escalating to emergencies requiring ER transfers.
- Enhanced Medical Capabilities: The behavioral health hospital was equipped with new supplies and equipment, such as those needed for evaluating female genitourinary issues and fetal health (e.g., fetal heart tone monitors and speculums). This enhancement allowed for onsite management of conditions that previously required ER visits.
- Improved Diagnostic Coordination: Coordination with laboratory and imaging services was enhanced to ensure rapid turnaround times for urgent evaluations. This improvement facilitated timely medical assessments and interventions, reducing the need for ER transfers.
- Early Patient Assessments: Patients were assessed earlier in their stay to identify and address medical concerns proactively, preventing escalation to emergencies.
Results
In the first three months of implementing these strategies, the behavioral health hospital saw a greater than 50% reduction in ER transfers, which equated to an average of $76,800 per month in direct cost savings.
This reduction has been maintained consistently over the past two years. This success can be attributed to the thorough training of nursing staff, effective triage protocols, enhanced onsite medical capabilities, and improved coordination with diagnostic services.
Conclusion
The partnership between the behavioral health hospital and the Med-X team demonstrates how a multidisciplinary, well-rounded approach can reduce avoidable ER transfers within a behavioral healthcare inpatient setting. By focusing on education, workflow improvements, and enhanced medical capabilities, we have been able to keep behavioral health care consistent, ease the load on emergency services, and ultimately lower healthcare costs. After two years of success, it’s clear this approach works and can be adapted elsewhere. Our collaboration highlights the power of working together for better healthcare outcomes.

References:
- Nordstrom K, Berlin J, Nash S, Shah S, Schmelzer N, Worley L (2023). Boarding of Mentally Ill Patients in Emergency Departments: American Psychiatric Association Resource Document). Psychiatry Online: https://doi.org/10.1176/appi.focus.23022001
- Brickman K and Silvestri J (2019). The emergency car emodel: A new paradigm for skilled nursing facilities. Geriatric Nursing 41 (2020) 242-247.
- Ingber M, Feng Z, Khatutski G, Wang J, Bercaw, L, Zheng N, Vadnais A, Coomer N, Segelman M (2017). Initiative to Reduce Avoidable Hospitalizations Among Nursing Facility Residents Showing Promising Results. Health Affairs 36(3). https://doi.org/10.1377/hlthaff.2016.1310
- Stadler D, Oliver B, Raymond J, Routzhan G, Flaherty E, Stahl J, Batsis J, Bartels S (2019). Reducing Avoidable Facility Transfers (RAFT): Outcomes of a Team Model to Minimize Unwarranted Emergency Care at Skilled Nursing Facilities. Journal of American Medical Directors Association 20(8): 929-934. https://doi.org/10.1016/j.jamda.2019.03.010